What are Social Determinants of Health?
Yet despite this spending, health outcomes in the U.S. are lacking. Average life expectancy has decreased for the second year in a row, maternal mortality rates are higher than most developed countries, our obesity rates continue to grow, and the proportion of Americans reporting fair or poor health has grown over the past 15 years.
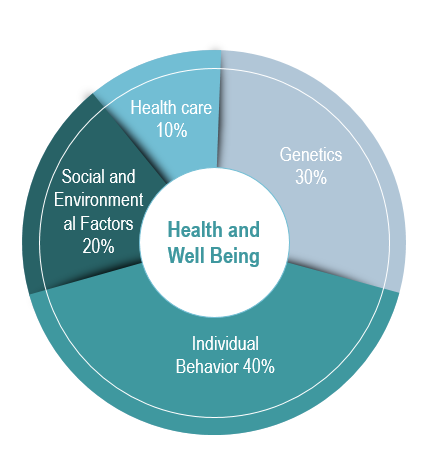
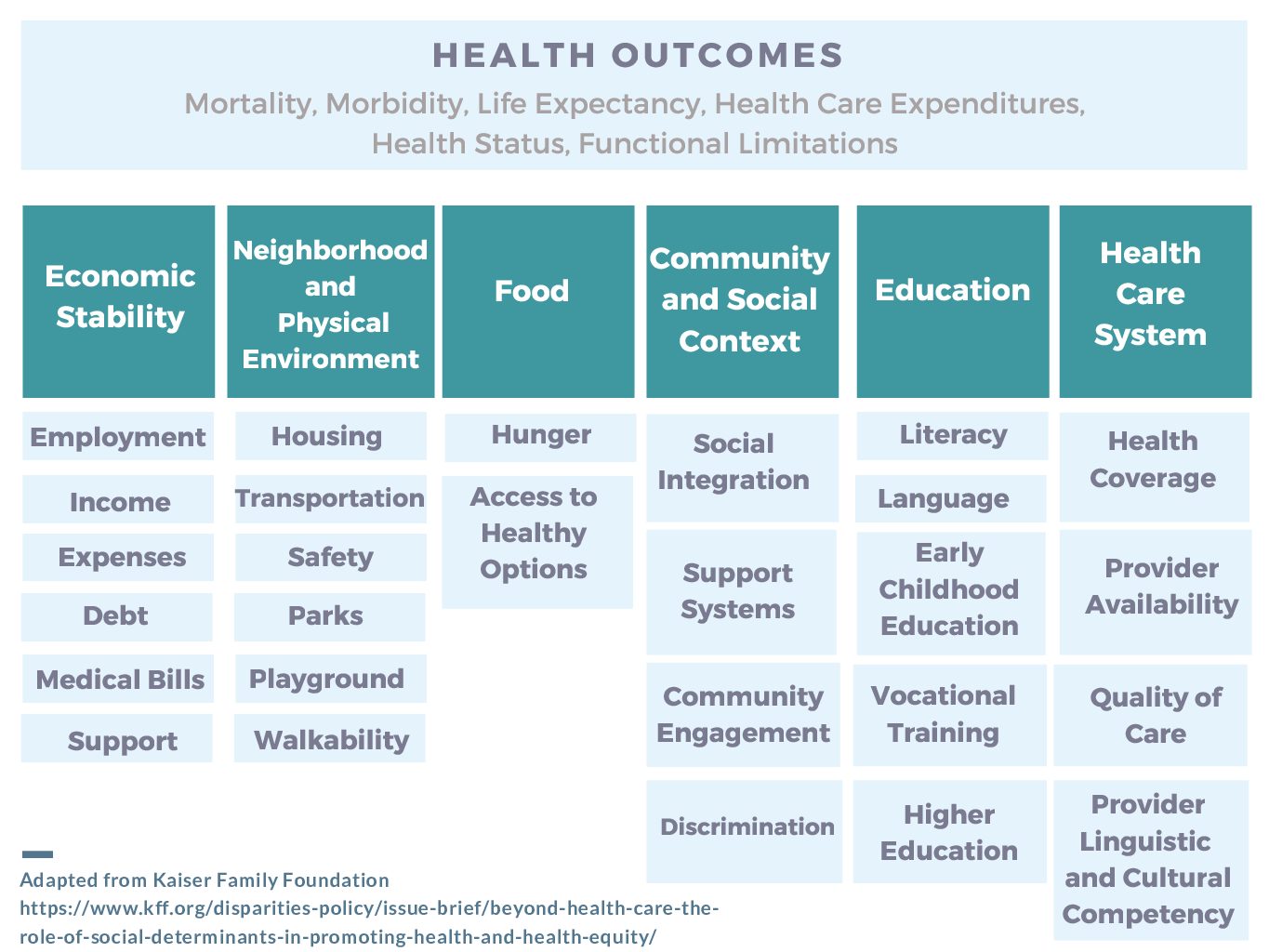
Although we spend trillions on health care every year, inadequate access to housing, proper nutrition, transportation, and factors such as education, employment, and diet and exercise can make a considerable impact on health. According to Brookings Institution, other developed nations spend far more on social services than on healthcare services, while in the U.S., we spend just 56 cents on social services for every dollar spent on healthcare. States also differ in their spending ratios, leading to differing outcomes; states with a higher ratio of social to health spending have significantly better health outcomes for such conditions as adult obesity, asthma, mental health indicators, mortality rates for lung cancer, high blood pressure, heart attacks, and Type 2 diabetes.
Healthy People 2020 >
The HHS Office of Disease Prevention and Health Promotion sponsors the Healthy People Initiative, an ongoing set of healthcare goals for the country’s healthcare system. Social determinants of health is a key objective as part of Healthy People 2020, which aims to “create social and physical environments that promote good health for all.” The website lists the government’s key objectives, as well as ongoing interventions, resources, and data.
Centers for Disease Control and Prevention >
The CDC has compiled a compendium of data about social determinants, as well as a list of CDC programs and policy resources to support efforts to address social determinants.
National Academy of Medicine >
National Academy of Medicine provides an overview of the role that social determinants play in health outcomes.
Kaiser Family Foundation >
Kaiser Family Foundation has published an issue brief describing the role of social determinants in promoting health and health equity, which includes data and previous efforts to integrate social determinants into healthcare services.
Robert Wood Johnson Foundation >
Social determinants of health are a focus area for RWJF; the foundation sponsors research and analysis supporting the topic.
The Commonwealth Fund wrote a review to help inform users of the Return on Investment (ROI) Calculator for Social Determinants of Health as a part of their review of evidence for health-related social needs interventions.
British Medical Journal, “Health and Social Services Expenditures: Associations with Health Outcomes.” >
Study assesses how health and social services spending impacts certain health outcomes, including life expectancy at birth, infant mortality, low birth weight, maternal mortality, and potential years of life lost. The study finds that health services spending is only associated with better health outcomes in two of the five measures, while higher social service spending improved health outcomes for three of the five indicators.
PLoS ONE, “Leveraging the Social Determinants of Health: What Works?” >
Study summarizes recent studies examining the impact of investments in social services or integrated health and human service models on health outcomes and healthcare spending. The study found that most studies found some significant positive effects on either health outcomes, costs, or both. Longer analysis available.
Barriers to Addressing Social Determinants
Complex Tapestry of Federal Programs and Services
- The federal government funds over 80 programs that provide aid to people with low incomes, ranging from programs that provide healthcare services, behavioral healthcare services, food benefits, cash assistance, transportation assistance, energy assistance, among many others.
- The authority, funding and administration of many of these programs was established and has evolved differently over time, creating a number of different programmatic siloes at the federal level, as well as at the state or local implementation level.
- While siloed programs create inefficiencies in program administration, more importantly, they also adversely impact Americans’ experiences and ability to access benefits and services.
- Siloes also have significant implications for efforts to better coordinate or integrate services as part of a whole-person approach – impeding attempts to blend funding across programs, or to innovate or modify the way in which services are delivered.
Below are some examples of commonly raised barriers:
Administrative
- Burdensome regulations and statutory requirements.
- Duplicative and complex reporting requirements, varying measures of success
- Lack of comprehensive central data systems for eligibility, tracking, etc.
- Difficulty in collecting data on social determinants from providers, also difficulty in connecting data from community based organizations to providers.
- Diffusion of responsibility and delivery systems – state, managed care organizations, Accountable Care organizations, providers, community health workers, human services departments, etc.
Consumer Experience
- Complex applications and eligibility processes, and multiple points of entry.
- Misaligned objectives and benefit cliffs, and little incentive to decrease use of programs.
- Varying requirements to maintain eligibility (e.g. work requirements) and in use of benefit.
